
1.4 Million Lawfully Present Immigrants May Lose Federal Medical Benefits
5 min read
A major change in federal law could soon disrupt health coverage for more than one million people. The recently passed One Big Beautiful Bill Act (H.R. 1) eliminates the long-standing federal option that allowed states to offer Medicaid and CHIP to certain lawfully present immigrants.
For the last 20 years, 37 states used this option to ensure children, pregnant people, and low-income adults could get essential health care. Now, that pathway is being removed.
Whether you’re a parent, a Medicaid enrollee, or someone helping others navigate benefits, understanding what this law changes and what steps you may need to take is key.
For ongoing updates about how federal laws affect your health, income, and family stability, visit BenefitKarma.com.
What the 2025 law actually changes
The OBBBA eliminates the federal “lawfully present” option that states have relied on since 2002. Under previous rules, states could choose to provide Medicaid and CHIP to immigrants who were lawfully present in the U.S., even if they did not qualify under the traditional, more restrictive federal categories.
With the elimination of this option:
States are no longer allowed to cover these immigrants through Medicaid or CHIP, even if they want to.
Coverage will end for groups who used this pathway, including children, pregnant people, and adults under Medicaid expansion.
Eligibility is narrowed to the older, stricter federal categories, which exclude many otherwise lawfully present individuals.
This is not an administrative interpretation. It is a statutory change, meaning states must comply.
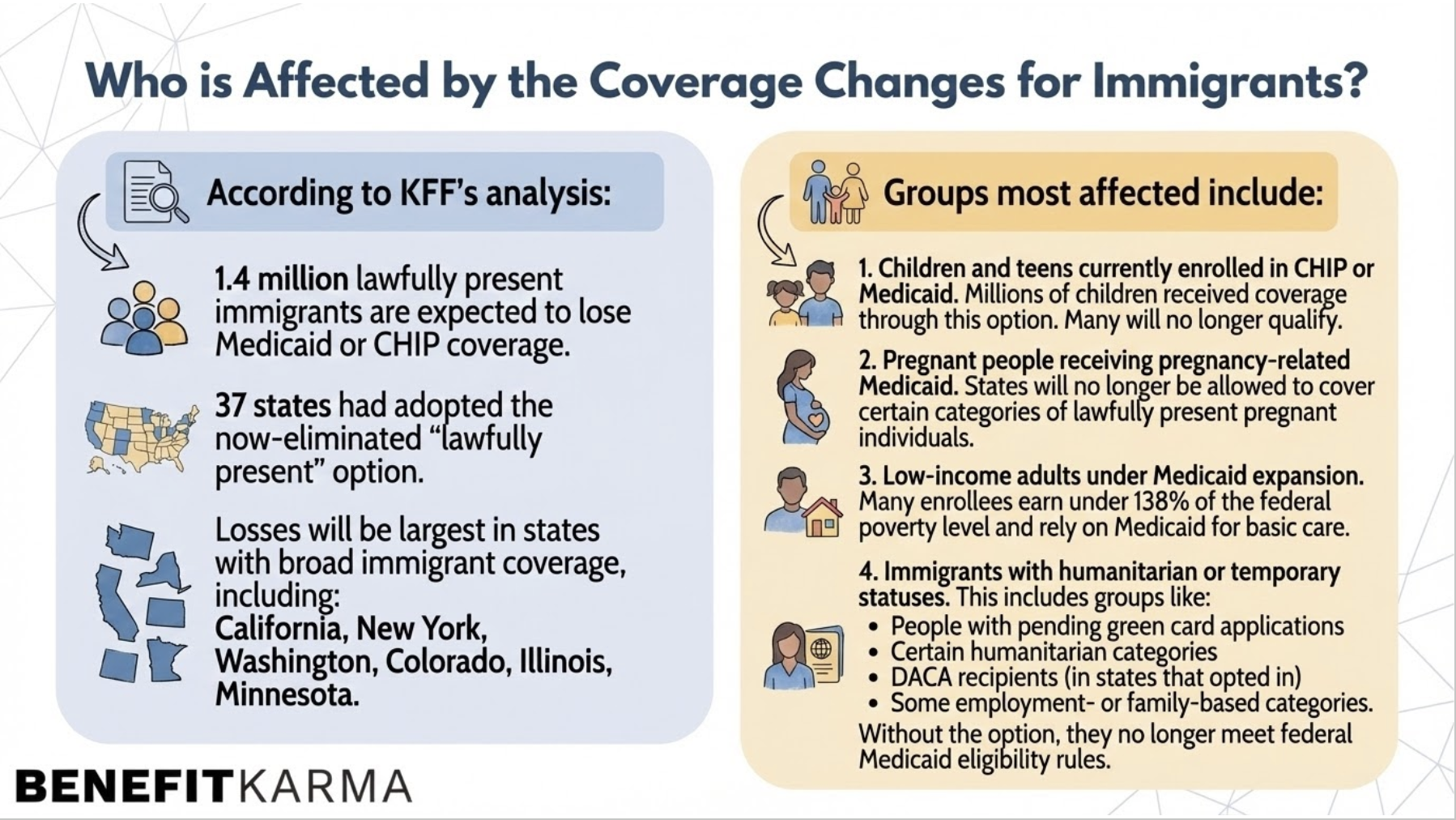
How many people lose coverage, and in which states?
According to Kaiser Family Foundation’s analysis:
1.4 million lawfully present immigrants are expected to lose Medicaid or CHIP coverage.
37 states had adopted the now-eliminated “lawfully present” option.
Losses will be largest in states with broad immigrant coverage, including:
California
New York
Washington
Colorado
Illinois
Minnesota
Groups most affected include:
1. Children and teens currently enrolled in CHIP or Medicaid
Millions of children received coverage through this option. Many will no longer qualify.
2. Pregnant people receiving pregnancy-related Medicaid
States will no longer be allowed to cover certain categories of lawfully present pregnant individuals.
3. Low-income adults under Medicaid expansion
Many enrollees earn under 138% of the federal poverty level and rely on Medicaid for basic care.
4. Immigrants with humanitarian or temporary statuses
This includes groups like:
People with pending green card applications
Certain humanitarian categories
DACA recipients (in states that opted in)
Some employment- or family-based categories
Without the option, they no longer meet federal Medicaid eligibility rules.
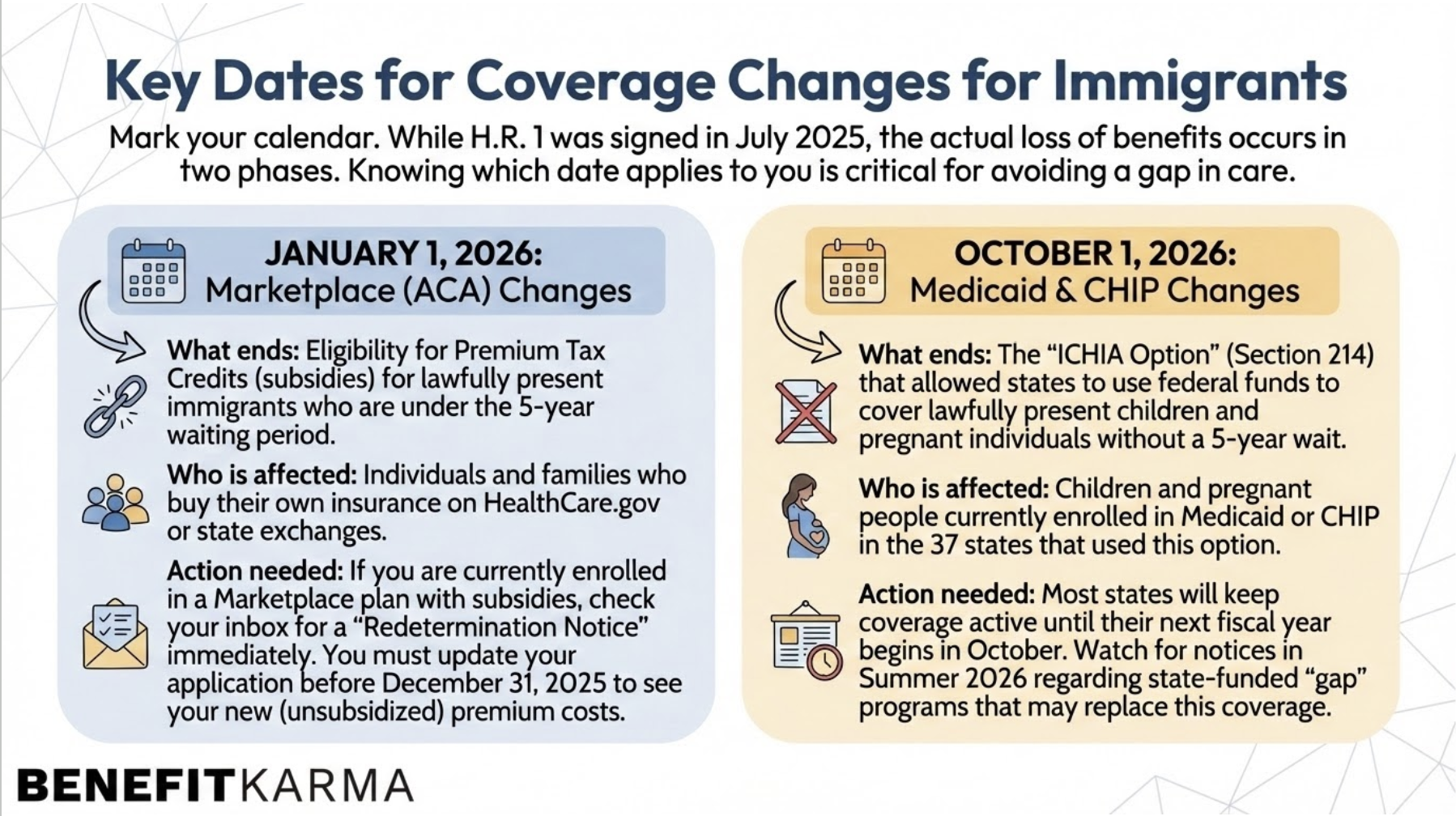
When coverage changes take effect
While exact timing depends on how states phase out the option, most people will experience changes:
At renewal, when they must reverify eligibility
When states update their Medicaid and CHIP systems to comply with federal law
Marketplace tax credit changes take effect January 1, 2026. However, the elimination of the Medicaid 'lawfully present' option officially takes effect in many states on October 1, 2026, though some states may restrict eligibility sooner. Check your specific state's timeline."
This means households should prepare now, not wait until benefits suddenly end.
What affected families should do right now
Here are the most important steps to protect yourself or help someone else prepare for immigrant benefits to change.
1. Check your Medicaid or CHIP renewal date
Renewal is the moment when eligibility changes are most likely to be applied.
2. Watch for notices from your state Medicaid agency
States are required to notify enrollees before making eligibility changes. Mail, email, and portal messages all count.
3. Explore Marketplace coverage options early
Many lawfully present immigrants qualify for significant subsidies, especially if their income is below 150% FPL.
Marketplace plans may offer:
Very low monthly premiums
Cost-sharing reductions for lower-income households
Coverage starting the first of the month after you enroll
Losing Medicaid or CHIP qualifies you for a Special Enrollment Period.
4. Review options for children
Children losing Medicaid or CHIP may still qualify for:
Low-cost Marketplace plans
State-funded programs (varies by state)
Community health centers with sliding-scale fees
5. Pregnant individuals should confirm coverage sources immediately
Pregnancy-related Medicaid eligibility will change for many categories previously covered.
Your state may:
Shift you to a narrower Medicaid category
Refer you to Marketplace coverage
Offer state-funded alternatives (in a few states)
6. Keep all immigration documentation updated
While this change is not about documentation problems, states may request verification during transitions.
7. Stay updated; states may create temporary programs
Some states are considering:
State-funded coverage
Gap programs for pregnant people
Continued coverage for children through state-only dollars
These programs vary widely, so staying informed is essential.
Bottom line
The OBBBA removes the federal authority that allowed states to cover lawfully present immigrants through Medicaid and CHIP. As a result, 1.4 million people (many of them children, pregnant individuals, and low-income families) are expected to lose public health insurance in the coming year.
If you or someone you know relies on this pathway, now is the time to review renewal dates, explore Marketplace options, and watch for official notices.